There has been extensive research to evaluate the relationship between television (TV) viewing and childhood overweight or obesity. Several cross-sectional studies have found an association between TV viewing and paediatric overweight or obesity(Reference Hume, Singh and Brug1–Reference Steffen, Dai and Fulton5), some studies have found no significant association(Reference Crooks6, Reference McMurray, Harrell and Deng7) while others have found a weak positive association(Reference Robinson8) or mixed results(Reference Anastassea-Vlachou, Fryssira-Kanioura and Papathanasiou-Klontza9, Reference Guillaume, Lapidus and Bjorntorp10). Several prospective studies have reported that there is a link between the amount of time TV is watched and overweight/obesity through different stages of the life course from early childhood to young adulthood(Reference Davison, Marshall and Birch11–Reference Viner and Cole17). The Framingham Children's Study found that children including pre-school children who watched the most TV had the greatest increases in body fat by early adolescence(Reference Proctor, Moore and Gao16). The 1958 British birth cohort(Reference Parsons, Manor and Power15, Reference Viner and Cole17) and New Zealand-based Dunedin birth cohort studies(Reference Erik Landhuis, Poulton and Welch12, Reference Hancox and Poulton13) both found childhood and adolescent TV watching to be prospectively associated with adult obesity. However, some studies have had small sample sizes(Reference Davison, Marshall and Birch11, Reference Proctor, Moore and Gao16), included only girls(Reference Davison, Marshall and Birch11) and relied upon self-reported BMI(Reference Kaur, Choi and Mayo14), and none of them has investigated change of TV viewing during the transition from the adolescent to young adulthood period and its impact on obesity.
One concern is whether children who reduce their sedentary behaviour significantly decrease their BMI(Reference Epstein, Paluch and Kilanowski18–Reference Gortmaker, Peterson and Wiecha20). A randomized controlled trial demonstrated that a reduction in TV viewing decreases BMI, waist circumference (WC) and waist-to-hip ratio (WHR) in schoolchildren(Reference Robinson21). Whether changes in TV viewing are associated with changes in BMI has not been assessed in observational studies, particularly whether changes in TV viewing pattern from adolescence to young adulthood are associated with subsequent changes in BMI, WC, WHR and obesity status in young adults.
Adolescence is arguably a critical period as habits, attitudes and physical morbidity that develop during adolescence may establish trajectories that have a profound influence on health and well-being in the long term(Reference Steinbeck, Baur and Cowell22). The transition from adolescence to young adulthood is characterized by the high continuity and incidence of obesity(Reference Gordon-Larsen, Adair and Nelson23). Evidence also supports that this transition marks a striking age-related physical activity decline(Reference Gordon-Larsen, Nelson and Popkin24, Reference Nelson, Gordon-Larsen and Adair25). Further, sedentary behaviour patterns such as TV viewing and computer use are increasing over time through the adolescent period(Reference Hardy, Bass and Booth26, Reference Nelson, Neumark-Sztainer and Hannan27). During the transition from adolescence to young adulthood, some adolescents might reduce their TV watching hours (e.g. enter into the labour market), some might continue with the same patterns and others might increase their TV watching hours. In the present prospective study we hypothesize that those adolescents who reduce their number of hours watching TV by young adulthood are less likely to become obese and that those who continue a longer duration or increase their TV watching hours have an increased level of obesity than those who persistently watch less hours of TV.
The primary aim of the study was to examine the prospective association between the change in TV watching patterns from adolescence to young adulthood and young adult BMI, WC, WHR and obesity. The secondary aim was to investigate the prospective association between patterns of TV watching and change in patterns of overweight from adolescence to young adulthood.
Methods
Study participants
The data are from the Mater–University of Queensland Study of Pregnancy and Its Outcomes (MUSP). MUSP is a prospective study of 7223 women and their offspring. Mothers received antenatal care at a major public hospital in Brisbane between 1981 and 1983 and delivered a live singleton child who was not adopted before leaving the hospital(Reference Najman, Bor and O'Callaghan28, Reference Keeping, Najman and Morrison29). Mothers and children have been followed up prospectively, with maternal questionnaires being administered at the first antenatal clinic visit, 3–5 d post-delivery, 6 months, 5, 14 and 21 years after birth. At 14 and 21 years, mothers and children were invited to the Mater Hospital where they completed a self-administered questionnaire and MUSP research staff undertook a physical assessment of a sub-sample of the participants including measurements of height and weight. For the present study, we have available data on TV watching at 14 and 21 years and measured height, weight, WC and WHR at 21 years for a sub-sample of 2439 participants. In general, participants lost to follow-up were more likely to be males and of Asian and Aboriginal/Torres Strait Islander background (all P < 0·001). Their mothers were more likely to be teenagers at the time of the first clinic visit, less educated, single or cohabitating, have three or more children, used tobacco and alcohol during pregnancy and be anxious and depressed at their first antenatal visit(Reference Najman, Bor and O'Callaghan28). Written informed consent from the mothers was obtained at all data collection phases and from the young adults at the 21 years follow-up. Ethics committees at the Mater Hospital and the University of Queensland approved each phase of the study.
Measurements of television watching
At the 14 and 21 years follow-ups, offspring reported the amount of time they spent watching TV during weekdays (from Monday to Friday) and weekend days (Saturday and Sunday) in separate questions with the same response options: ‘never watched TV’, ‘less than 1 hour’, ‘1 to less than 3 hours’, ‘3 to less than 5 hours’, ‘5 to less than 7 hours’ and ‘7 hours or more’. Although virtually an international recommendation is that children should spend no more than 2 h/d on screen-based leisure activities(Reference Grontved and Hu30), in our study using the available information we categorized the TV watching hours into ‘less than 3 hours’ and/or ‘3 or more hours per day’. We collapsed six response options into two categories: <3 h/d and/or ≥3 h/d. A composite indicator of TV watching at 14 and 21 years was generated as follows: (i) TV watched <3 h/d at 14 and 21 years; (ii) TV watched <3 h/d at 14 years but ≥3 h/d at 21 years; (iii) TV watched ≥3 h/d at 14 years but <3 h/d at 21 years; and (iv) TV watched ≥3 h/d at 14 and 21 years. For the main analysis we used TV watching during the weekdays as an exposure as we believe this provides overall distribution of the TV watching time for the adolescents and young adults. However, we repeated the analysis using TV watching during weekend days.
Measurement of BMI, waist circumference and waist-to-hip ratio
At the 14 and 21 years follow-ups, offspring's height was measured without shoes using a portable stadiometer to the nearest centimetre. His/her weight was measured in light clothing with a scale accurate to 0·2 kg. Two measures of weight were taken with a 5 min interval and the mean of these two measures was used in all analyses. At 21 years, WC was measured horizontally using a tape (provided by Sullivans Haberdashery & Craft Wholesalers, Australia) roughly in line with the participant's navel or belly button, directly against the skin without compressing the skin. The average of the two measures was taken. Similarly, the hip measure was repeated twice and the average was taken. The participant was asked to lower the tape measure down to the hips following the same procedure, ensuring the measurement was taken from the point of greatest width. If the tape measure was not around the point of greatest width, the interviewer simply asked the participant to lower or raise the tape. Adolescents’ BMI (weight in kilograms divided by the square of height in metres, i.e. kg/m2) was calculated based on measured height and weight at the 14 years follow-up and BMI was categorized as normal or overweight according to standard definitions derived from international surveys by Cole et al.(Reference Cole, Bellizzi and Flegal31). At 21 years, BMI was categorized into normal (<25 kg/m2), overweight (25–29 kg/m2) and obese (≥30 kg/m2) using the WHO classification of BMI cut-offs(32). WC was categorized for males as follows: <94 cm as normal, 94–<102 cm as overweight and ≥102 cm as obese; and for females as follows: <80 cm as normal, 80–<88 cm as overweight and ≥88 cm as obese(33). WHR was categorized for males as follows: <0·90 as normal, 0·90–<1·00 as overweight and ≥1·00 as obese; and for females as follows: <0·80 as normal, 0·80–<0·85 as overweight and ≥0·85 as obese(33).
Measurement of confounding factors
The factors we considered to be potential confounding factors were on the basis of a priori knowledge(Reference Hernan, Hernandez-Diaz and Werler34) of their association with TV watching (exposure) and BMI, WC and WHR (outcomes). We also relied on the published literature where potential confounders for these associations have been identified, examined and discussed(Reference Grontved and Hu30, Reference Ekelund, Brage and Froberg35, Reference Hu, Li and Colditz36). Potential confounders we considered were child age (in years) at the 14 years follow-up, maternal educational attainment (did not complete secondary school, completed secondary school, completed further/higher education), parental racial origin (White, Asian and Aboriginal-Islander) and maternal pre-pregnancy BMI. These data were obtained from questionnaires at the first clinic visit and obstetric records. Maternal pre-pregnancy BMI was calculated based on maternal measured height at pregnancy and self-reported pre-pregnancy weight, which was recorded at the study initiation from maternal questionnaires. A high degree of correlation was obtained between maternal estimate of her pre-pregnancy weight and her measured weight on the first antenatal visit (Pearson's correlation coefficient = 0·95). Further confounders we considered were frequency of consumption of fast food and soft drinks, family attitude to having meals together, sports and behavioural problems (using the Child Behavioral Check List(Reference Achenbach37)) at 14 years follow-up. At the 14 years follow-up mothers were asked to report the frequency of their child's consumption of fast food and soft drinks (all with response options of ‘rarely or never’, ‘at least 2 or 3 times a week’, ‘most days’), family attitude to having meals together (‘at least once a day’, ‘few times/once/less than once a week’) and to report the amount of time children spent on sports or exercise (‘4–7 days per week’, ‘0–3 days per week’). In addition, we had data for total recreational time based on total hours of computer use and Internet use in the last week at the 21 years follow-up.
Statistical analysis
The adolescents’ and young adults’ TV watching patterns and their average BMI, WC and WHR by daily hours of TV watching are presented as descriptive analyses. We examined the bivariate association between TV watching patterns from 14 to 21 years and potential confounding factors. We used a χ 2 test when the covariate was categorical and an F test when it was continuous. Statistical evidence for a difference in effect between males and females was assessed by computing a likelihood ratio test of the interaction with sex. As we found no statistical evidence that the effect differed between the sexes, results are presented for males and females combined.
A series of multiple linear regression models was used to determine the adjusted mean of BMI, WC and WHR by TV watching patterns in four mutually exclusive categories taking into account potential confounding factors. As we found adjustment for potential confounding factors (as listed above) did not alter the associations substantially, we present only the fully adjusted mean values in Fig. 1. Similarly, a series of multinomial regression models was used to assess the association between offspring's TV watching patterns in the same four mutually exclusive categories and young adults being normal, overweight or obese at age 21 years based on BMI, WC and WHR categories (see footnote of Table 3 for a description of the different models). Finally, using a series of multinomial regression models we examined the prospective association between patterns of TV watching with patterns of overweight categories from adolescence to young adulthood. BMI at 21 years was grouped as normal or overweight (including obese category). The pattern of BMI from 14 to 21 years was grouped into four categories as: (i) normal at 14 and 21 years; (ii) normal at 14 years but overweight at 21 years; (iii) overweight at 14 years but normal at 21 years; and (iv) overweight at 14 and 21 years.
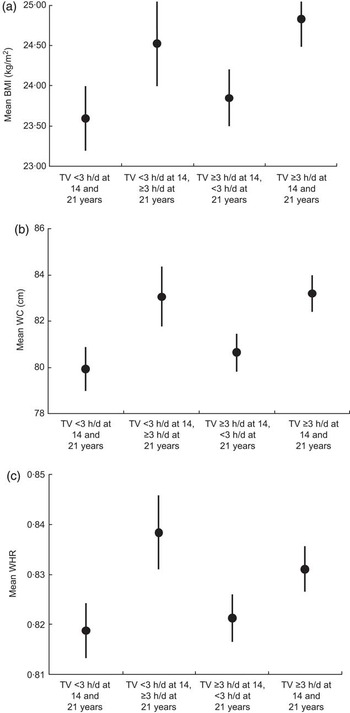
Fig. 1 Adjusted (a) BMI, (b) waist circumference (WC) and (c) waist-to-hip ratio (WHR) at 21 years by television (TV) watching patterns at 14 and 21 years; sub-sample of 2439 offspring in the Mater-University of Queensland Study of Pregnancy (MUSP) Cohort, Brisbane, Australia. Values are means with their 95 % confidence intervals represented by vertical bars
All analyses were undertaken using the STATA statistical software package version 11·0 (StataCorp, College Station, TX, USA).
Results
The mean BMI at 14 years was 20·59 (sd 3·66) kg/m2. The mean BMI, WC and WHR for young adults at 21 years were 24·20 (sd 4·88) kg/m2, 81·64 (sd 12·21) cm and 0·83 (sd 0·60), respectively. Of the 2439 young adults, 21·39 % were overweight and 11·96 % were obese at age 21 years. While at 14 years 35·67 % of adolescents watched TV for <3 h/d, the corresponding percentage was 50·59 % for young adults. Of all offspring, nearly one in four (23·00 %) watched TV for <3 h/d at 14 and 21 years; 12·67 % watched TV for <3 h/d at 14 years but for ≥3 h/d at 21 years; 30·59 % watched TV for ≥3 h/d at 14 years but for <3 h/d at 21 years; and a third (33·74 %) watched TV for ≥3 h/d at 14 and 21 years (Table 1).
Table 1 Adolescents’ and young adults’ TV watching and anthropometry; sub-sample of 2439 offspring in the Mater–University of Queensland Study of Pregnancy (MUSP) Cohort, Brisbane, Australia

TV, television; WC, waist circumference; WHR, waist-to-hip ratio.
*P value indicates the significance level of the difference in mean BMI, WC and WHR by TV watching categories (using an F test).
The associations between TV watching patterns at age 14 and 21 years and family, maternal and child characteristics are presented in Table 2. Offspring whose mothers did not complete secondary school, with Aboriginal-Islander parents, with mothers who were obese before the index pregnancy, with mothers who reported not eating family meals together, who were male, consumed soft drinks and had behavioural problems were at greater risk of spending more time watching TV consistently at adolescence and young adulthood (all P < 0·05).
Table 2 Association of adolescents’ and young adults’ TV watching patterns with family, maternal and child characteristics; sub-sample of 2439 offspring in the Mater–University of Queensland Study of Pregnancy (MUSP) Cohort, Brisbane, Australia

TV, television.
*P value indicates the significance level of the difference between TV watching at 14 and 21 years with family, maternal and offspring characteristics (using an F test for continuous data and a χ 2 test for categorical data).
Adjusted mean BMI, WC and WHR by TV watching patterns at 14 and 21 years are presented in Fig. 1. Those offspring who watched TV for <3 h/d at 14 years but for ≥3 h/d at 21 years or who watched TV for ≥3 h/d at 14 and 21 years had greater BMI, WC and WHR at 21 years than those who consistently watched TV for <3 h/d at 14 and 21 years. In contrast, those offspring who watched TV for ≥3 h/d at 14 years but <3 h/d at 21 years had similar mean BMI, WC and WHR at 21 years to those who persistently watched TV for <3 h/d at 14 and 21 years. This association remained independent of potential confounding factors including child gender, age, maternal education, racial origin, BMI, family meals, sports and fast-food behaviours (unadjusted mean values not presented in Fig. 1).
Unadjusted and adjusted odds of being overweight and obese (using the BMI, WC and WHR cut-off) at age 21 years by TV watching patterns at 14 and 21 years are presented in Table 3. In the fully adjusted model, the odds of being obese at 21 years was 2·33 (95 % CI 1·41, 3·85) for those who watched TV for <3 h/d at 14 years but for ≥3 h/d at 21 years compared with those who reported TV watching <3 h/d at 14 and 21 years. Similarly, for those who reported TV watching ≥3 h/d at 14 and 21 years, their odds of being obese at 21 years were 2·31 (95 % CI 1·52, 3·51). These associations were independent of potential confounding factors. The strength and direction of the associations remained similar to those observed for BMI categories whether using WC or WHR categories of normal, overweight and obese.
Table 3 Risk (odds ratios with 95 % confidence intervals) of overweight and obesity at 21 years by TV watching patterns at 14 and 21 years, adjusted for offspring, maternal and family factors (n 2176); sub-sample of offspring in the Mater–University of Queensland Study of Pregnancy (MUSP) Cohort, Brisbane, Australia

TV, television; WC, waist circumference; WHR, waist-to-hip ratio.
Model 1: unadjusted.
Model 2: model 1+child's gender and age at 14 years.
Model 3: model 2+maternal education, racial origin and BMI.
Model 4: model 3+family meals, fast food, soft drinks, sports and child behavioural problems.
In additional analyses, we examined whether TV watching pattern predicted overweight pattern from 14 to 21 years (Table 4). In the fully adjusted model, we found that the odds of being normal weight at 14 years but overweight at 21 years was 4·30 (95 % CI 1·43, 12·90) times higher for those who watched TV for <3 h/d at 14 years but for ≥3 h/d at 21 years compared with those who maintained healthy BMI and watched TV for <3 h/d at both times. The odds of becoming overweight at 21 years was 2·49 (95 % CI 0·90, 6·91) for those who persistently watched TV for ≥3 h/d at 14 and 21 years compared with their counterparts who maintained healthy BMI and watched TV for <3 h/d at both times. In the additional analyses when we repeated all analyses adjusting for time spent for recreational purposes during the last week, we found that the associations remained consistent (results not shown).
Table 4 Prospective association (odds ratios with 95 % confidence intervals) of TV watching patterns with BMI categories from adolescence to young adulthood (n 1873); sub-sample of offspring in the Mater–University of Queensland Study of Pregnancy (MUSP) Cohort, Brisbane, Australia

TV, television.
Model 1: unadjusted.
Model 2: model 1+child's gender and age at 14 years.
Model 3: model 2+maternal education, racial origin and BMI.
Model 4: model 3+family meals, fast food, soft drinks, sports and child behavioural problems.
Discussion
In a large population sample of adolescents, those who reduced their TV watching hours from adolescence to young adulthood had similar mean BMI, WHR and WC at 21 years to those who consistently watched less TV at both 14 and 21 years. Similarly, those offspring who persistently watched TV for longer at 14 and 21 years as well as those who watched less TV at 14 years but increased their TV watching at 21 years had greater BMI, WHR and WC at 21 years than those who consistently watched TV for a shorter duration during this transitional period in their life. This association remained strong and consistent after adjusting for potential confounding factors such as child gender, age, maternal education, racial origin, sports activity, fast-food behaviours, recreational time spent in computer and Internet use, maternal BMI and family meals. Findings of the study suggest that adolescents who cut their TV watching hours by young adulthood are at less risk of becoming obese and those adolescents who continue or increase their TV watching hours are at greater risk of higher BMI, WC, WHR and obesity by young adulthood.
To our knowledge, the present study is the first longitudinal study that has focused on changes in TV viewing time in adolescents and young adults and the impact of these changes on obesity status in young adults. Although previous longitudinal studies have shown a significant relationship between TV viewing and the development of obesity in older children(Reference Erik Landhuis, Poulton and Welch12, Reference Hancox and Poulton13, Reference Parsons, Manor and Power15, Reference Viner and Cole17), none has examined the effect of change in TV viewing time in adolescence through young adulthood on overweight/obesity in young adults. Although a few intervention studies support the notion that reducing TV viewing may reduce the risk of obesity in children(Reference Gortmaker, Peterson and Wiecha20, Reference Robinson21), these studies were conducted in schoolchildren. There is a need to know whether the same findings are observed in a population sample of adolescents becoming young adults.
Investigators have hypothesized that TV viewing may cause obesity by one or more of three mechanisms: (i) reduced or displacement from physical activity; (ii) increased energy intake while watching TV or the effects of food advertising on unhealthy food consumption; and (iii) reduced inactive metabolic rate(Reference Robinson38). The first hypothesis suggests that TV watching and other sedentary behaviours displace physical activity. According to this hypothesis, increased time spent inactive is suggested to be a primary factor contributing to the current increases in obesity seen in adolescents(Reference Dietz and Gortmaker39, Reference Gortmaker, Must and Sobol40) because inactivity is associated with low energy expenditure. TV viewing is thought to predict unhealthy food preferences and dietary behaviours that continue until young adulthood(Reference Harris and Bargh41). There is increased consumption of energy-dense snacks when meals are combined with TV viewing(Reference Coon, Goldberg and Rogers42, Reference Blass, Anderson and Kirkorian43). Also, there is some evidence that advertising on TV influences food consumption patterns, thus leading to adiposity(44). TV viewing has a profound lowering effect on metabolic rate and this may be a mechanism for the relationship between obesity and amount of TV viewing(Reference Klesges, Shelton and Klesges45). Hence, it is possible that reducing TV viewing could affect energy intake by minimizing cues to eat and by decreasing exposure to TV advertising. Also, it is possible that reductions in TV viewing result in increased energy expenditure via more low-intensity activity.
It is important to acknowledge some limitations to the present study. The loss to follow-up in the MUSP cohort was considerable. However, our results would be biased if the associations we have assessed were non-existent or in the opposite direction in non-participants; that is to say, if among non-responders those young adults who became obese were less likely to have greater adolescent BMI, which is unlikely. A variety of modelling strategies have been used in MUSP studies in order to adjust for attrition, although use of these methods has not resulted in marked alteration of findings(Reference Najman, Bor and O'Callaghan28, Reference Alati, Al Mamun and O'Callaghan46, Reference Al Mamun, Lawlor and Alati47). From our recent investigation, we found that the proportion lost to follow-up in MUSP is consistent with that in other large life-course cohorts (e.g. the British 1958 birth cohort(Reference Power and Elliott48) and the Avon Longitudinal Study of Parents and Children(Reference Blair, Drewett and Emmett49)). We also found broad similarities between our published findings and those of previous birth cohort studies (with shorter follow-ups) with lower attrition rates, providing some support that our findings may not be biased by loss to follow-up.
We compared our estimates of overweight at age 12–15 years and 20–24 years with those reported in the Australian National Nutritional Survey 1995 for similar age categories. At 14 years the prevalence of overweight was 25 % in MUSP; at age 21 years, it was 34 %. At age 10–14 years the prevalence of overweight in the Australian national survey was 22 % and at age 20–24 years it was the same (34 %)(Reference Booth, Wake and Armstrong50). We also compared the average TV viewing hours estimated in MUSP with the average an Australian adult spends. On average an Australian adult watches 22 h of TV/week per person(51), which is comparable to our estimate of 21 h/week per person at 21 years.
The reliability and validity of the self-reported TV viewing by the adolescents and young adults are questionable. A systematic review focusing on the measurement of TV viewing among children and adolescents reported that most multicomponent surveys (including cross-sectional and longitudinal studies) have used a single item to assess TV viewing(Reference Bryant, Lucove and Evenson52). The review identified only two studies(Reference Schmitz, Harnack and Fulton53, Reference Vilhjalmsson and Thorlindsson54) that evaluated reliability and validity of self-reported TV viewing. One study(Reference Schmitz, Harnack and Fulton53) compared self-reported weekday TV viewing with self-reported weekly TV viewing diaries and found a moderate correlation (r = 0·5) and fair reliability for the same item one week apart (test–retest r = 0·34). The other study(Reference Vilhjalmsson and Thorlindsson54) reported poor negative correlations with its TV exposure item and a self-reported physical activity questionnaire (r = −0·06). In our study, we found a negative correlation of r = −0·08 between adolescents’ TV viewing and their sports participation. We also found another recent study for an adult population that compared self-reported TV viewing time with an objective measure obtained by an electronic TV monitor(Reference Otten, Littenberg and Harvey-Berino55). That study found respondents underestimated their TV viewing time by only 36 min/d on average and large errors were rare in the sample, which suggests that simple self-report measures may be appropriate to study TV viewing behaviour in many settings, especially at the population level. Like many cohort studies, in MUSP we have collected a great deal of data at different follow-ups of the study. Some of the data were simply collected as part of the broader coverage of lifestyle factors such as TV watching at the 14 years follow-up. At that time, we did not asses the reliability and validity of these measurements. These are self-reported data with a possibility of reporting bias. However, the existing evidence supports that our data may not provide any substantial bias in the study.
Systematic reviews and meta-analyses found that the strength of statistically significant associations between children's/adolescents’ TV viewing and obesity is likely to be too small to be of substantial clinical relevance(Reference Marshall, Biddle and Gorely56). A recent meta-analysis for an adult population also found that prolonged TV viewing was associated with increased risk of type 2 diabetes, CVD and all-cause mortality but the effect size was relatively small(Reference Grontved and Hu30). This suggests that the strength of association we observed is consistent with published articles.
Conclusions
In a population-based birth cohort, we found that those who reduced their TV watching hours during the transition from adolescence to young adulthood were at less risk to become obese and that those who continued or increased their TV watching hours were at greater risk to become obese. The study findings support the notion that reduction of sedentary activities including TV watching would reduce the obesity status in our community. Our efforts to decrease obesity by reducing TV watching hours among adults should consider interventions to reduce TV time among adolescents. Attempts to reduce adult obesity by modifying TV viewing habits need to begin in early adolescence. Further studies are needed to evaluate the extent to which these changes persist over a longer period.
Acknowledgements
The study was funded by the National Heart Foundation of Australia (ID 2007001895) and the University of Queensland Foundation Research Excellence Awards. The core MUSP study was funded by the National Health and Medical Research Council (NHMRC) of Australia. A.A.M. is funded by the NHMRC Career Development Awards in Population Health (ID 519756). The views expressed in this paper are those of the authors and not necessarily those of any funding body. There is no conflict of interest. A.A.M. initiated the concept, conducted the analyses and drafted the initial manuscript; all co-authors interpreted the results and critically revised the manuscript. The authors thank all participants in the study, the MUSP data collection team and Greg Shuttlewood, University of Queensland who helped manage the data for MUSP.









